
Therapy Intake Assessment Template
Key Takeaways
- Therapy intake assessments are crucial for effective treatment planning.
- They help mental health professionals gather essential information about new clients.
- A therapy intake assessment template streamlines the intake process and ensures consistency.
What Is a Therapy Intake Assessment Note?
A therapy intake assessment note is a structured document used by mental health professionals to collect and organize information about a new client during the initial intake assessment. This note serves as a foundation for understanding the client's background, current symptoms, and treatment goals.
The therapy intake assessment note is an essential tool in the therapeutic relationship. It aids in developing a personalized treatment plan by capturing details about the client's mental health history, family history, medical history, and any previous diagnoses. By using a therapy intake assessment template, practitioners can ensure they don't miss any critical information during the assessment process.
Key Components of a Therapy Intake Assessment Note
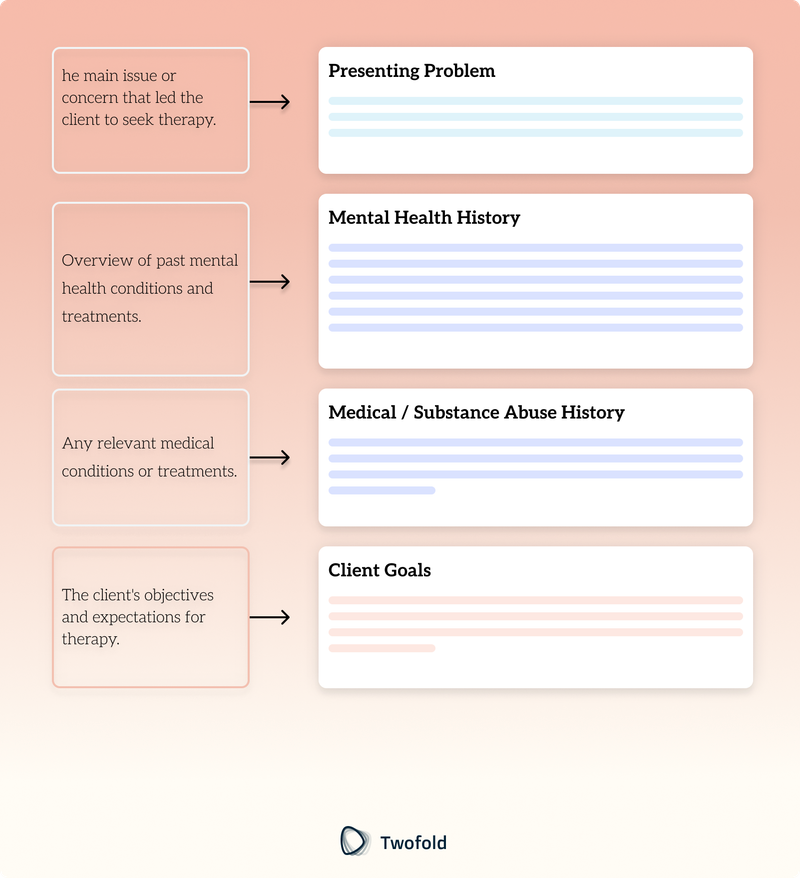
A therapy intake assessment note typically includes the following components:
- Client Information: Basic details such as name, age, and contact information.
- Presenting Problem: The main issue or concern that led the client to seek therapy.
- Mental Health History: Overview of past mental health conditions and treatments.
- Family Mental Health History: Information about mental health conditions within the family.
- Medical History: Any relevant medical conditions or treatments.
- Substance Use: Details about the client's use of alcohol, drugs, or other substances.
- Risk Factors: Assessment of any potential risks, such as self-harm or substance abuse.
- Client's Goals: The client's objectives and expectations for therapy.
- Support System: Information about the client's social support network.
How to Use a Therapy Intake Assessment Template: Step-by-Step Process
Step 1: Gather Basic Client Information
Begin by collecting the client's basic information, including their name, age, contact details, and emergency contact information.
Step 2: Identify the Presenting Problem
Discuss with the client the primary reason for seeking therapy and document their main concerns and symptoms.
Step 3: Review Mental Health and Medical History
Ask the client about their past mental health conditions, treatments, and any relevant medical history to understand their background better.
Step 4: Assess for Risk Factors
Evaluate any potential risks, such as self‑harm or substance abuse, and discuss these openly with the client.
Step 5: Set Treatment Goals
Work with the client to establish clear treatment goals and expectations for future sessions.
Step 6: Document Support System
Record information about the client's support network, including family, friends, and other mental health professionals involved in their care.
Benefits of a Therapy Intake Assessment
Benefit | Description |
|---|---|
Consistency | Ensures all essential information is collected uniformly across clients. |
Efficiency | Streamlines the intake process, saving time for both clients and therapists. |
Comprehensive Understanding | Provides a solid foundation for developing effective treatment plans. |
Improved Communication | Facilitates better communication between mental health professionals. |
Example of a Therapy Intake Assessment Template
A well‑structured therapy intake assessment template is a valuable tool for mental health practitioners. It helps ensure that no critical information is overlooked during the initial assessment, setting the stage for successful treatment planning. Explore our example template to see how it can enhance your practice.
How to Customize a Therapy Intake Note?
Customizing a therapy intake note allows mental health professionals to tailor the document to the specific needs of their practice and clients. Consider incorporating additional sections relevant to your therapeutic approach or client demographics. Regularly review and update the template to reflect any changes in best practices or legal requirements.
Legal Compliance and Therapy Intake Assessments
Therapy intake assessments must adhere to legal and ethical standards to protect client confidentiality and ensure informed consent. Mental health professionals should be familiar with relevant laws and regulations, such as HIPAA in the United States, which governs the privacy and security of client information.
Additionally, documentation should be clear, accurate, and stored securely to maintain professional standards and support the therapeutic process. Regular training and updates on legal compliance are essential for practitioners to stay informed and provide the highest level of care.
Conclusion
A therapy intake assessment is a crucial step in the therapeutic process, providing a comprehensive overview of the client's mental health history and current needs. By using a therapy intake assessment template, mental health professionals can streamline the intake process, ensuring consistency and efficiency. This foundational step paves the way for effective treatment planning and a successful therapeutic relationship.
For advanced solutions in medical documentation, explore our AI medical scribe services, designed to revolutionize how you create and manage your clinical notes.
Disclaimer: This article is for informational purposes only and does not constitute legal or medical advice. Always consult professional guidelines and regulatory bodies for specific compliance requirements.
Frequently Asked Questions
Reduce burnout,
improve patient care.
Join thousands of clinicians already using AI to become more efficient.
Cognitive Distortions Worksheet Template
Discover practical Cognitive Distortions Worksheet templates to enhance your documentation efficiency.

Attendance Log Template
Discover practical Attendance Log templates to enhance your documentation efficiency.
Patient Education Handout Template
Discover practical Patient Education Handout Template templates to enhance your documentation efficiency.

