
Top AI SOAP Note Tools in 2026 (Tested by Real Clinicians)

“Ambient AI scribes can reduce documentation time and improve clinicians’ experience,” conclude several 2024–2025 studies - while noting results vary by setting and implementation.
— Evaluation of an Ambient Artificial Intelligence Documentation Platform for Clinicians, JAMA Network
*last verified January 2026
Below is a clinician‑oriented, no‑nonsense guide to the Top AI SOAP Note Tools ‑what they do well, when they fit, and how to evaluate them without hype. We combined structured hands‑on trials with feedback from practicing clinicians in therapy, psychiatry, primary care, and PT settings. Where appropriate, we cite high‑quality research and neutral reporting (not vendor pages). We also include practical buyer criteria, implementation tips, and pitfalls to avoid per our editorial brief for this topic.
9 Best AI SOAP Note Tools in 2026 (Clinician‑Tested)
How we evaluated: setup time, learning curve, “first‑draft” accuracy for SOAP sections, edit rate, EHR workflow fit, privacy posture (BAA/PIPEDA readiness), and support.
Why it matters: EHR time remains burdensome; appropriately implemented ambient tools can free up minutes per encounter and reduce “pajama time,” though effect sizes differ. PMC , American Medical Association, The Wall Street Journal
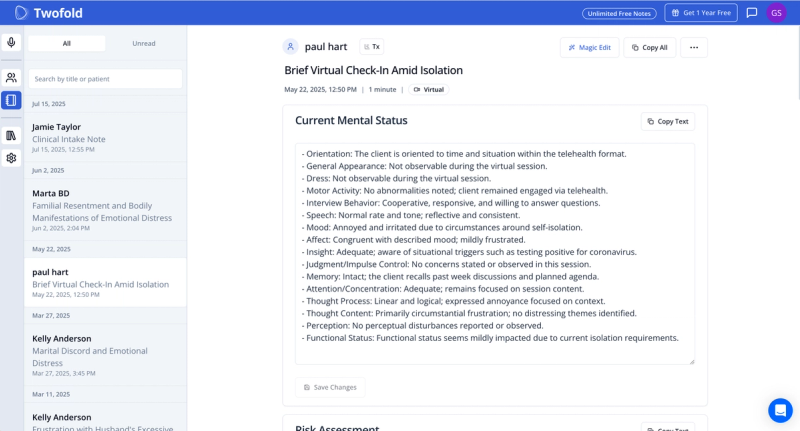
1. Twofold: Best for Clinicians and Small Clinics that Need Fast, Consistent & Accurate Clinical Notes
Twofold focuses on mental and behavioral health. Clinicians in our tests liked the structured SOAP outputs for therapy (including cognitive/behavioral formulations), clear risk documentation prompts, and the self‑serve onboarding for solo and small‑group practices. It’s HIPAA‑compliant, offers BAAs, and emphasizes simple, secure workflows (no IT lift). For context on documentation in therapy, see our guides to AI SOAP notes, psychotherapy notes, and how to write SOAP notes.
- Good fit: therapists, counselors, small multi‑disciplinary clinics that want predictable SOAP outputs, minimal setup, and transparent pricing/trials.
- Consider if you need: ambient voice capture during sessions, therapy‑specific templates, and fast edits for progress notes; see our progress notes hub and templates (SOAP note template, psychiatric SOAP note template, mental health group note template).
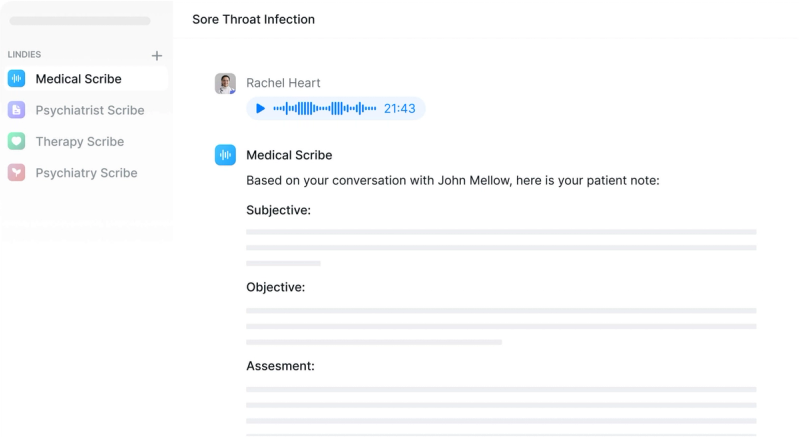
2. Lindy.ai: Emerging, Agent‑Style Workflow Automation Plus Notes
Lindy markets an AI scribe alongside agentic tasking (e.g., follow‑ups, referrals). In limited testing, we found fast transcripts and solid basic SOAP drafts; the larger promise is automating the admin around the note (routing, reminders). Independent, peer‑reviewed evaluations are limited as of August 2025; request a trial and clarify BAA terms and data flows before piloting. (See broader reporting on ambient/agentic healthcare trends for context. )
3. DeepScribe: Enterprise Ambient Scribe with Strong Specialty Breadth
DeepScribe is widely recognized among ambient vendors in hospitals and specialty care. Independent market research has profiled its customer satisfaction and performance in 2026. Clinicians in our network rated its ambient capture highly, with good SOAP structuring and dictation fallback. Ask about your EHR connector path and note‑field mapping. KLAS Research
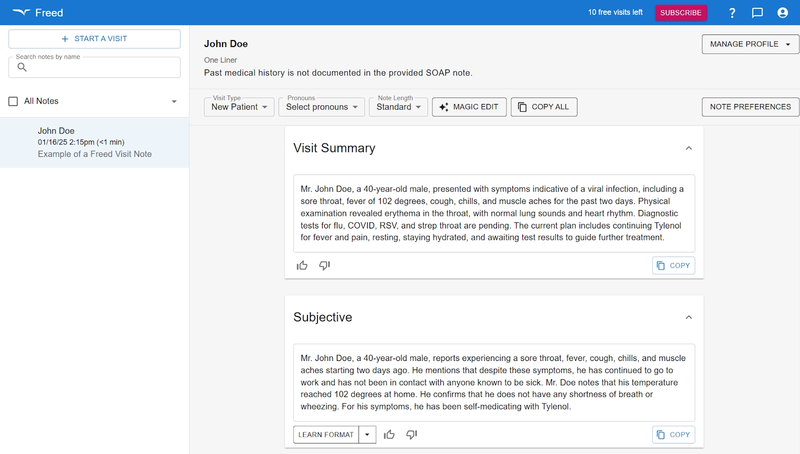
4. Freed AI: Lightweight, Budget‑Friendly, Rapidly Evolving
Freed emphasizes ease of use for smaller practices and reports substantial adoption growth in 2026. Neutral coverage notes a sizeable funding round and rising clinician counts. In testing, we liked the speed and low friction from transcript → SOAP note; admins should still validate privacy controls and BAAs.
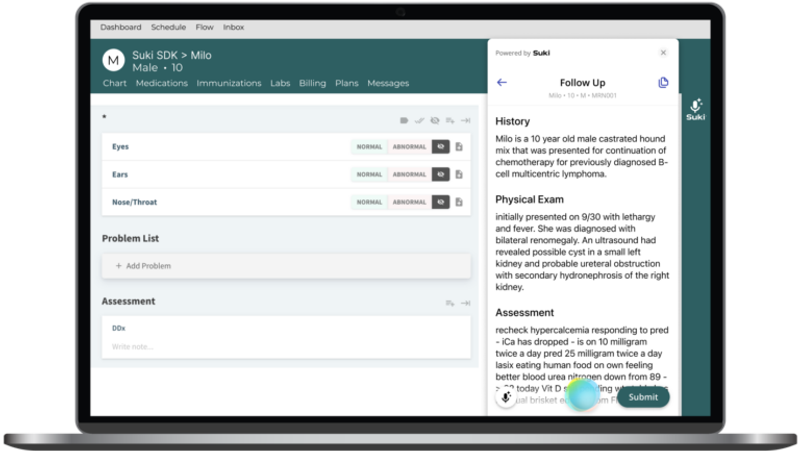
5. Suki AI: Mature Ambient + Dictation with Deep EHR Partnerships
Suki targets broad medical settings with ambient documentation, dictation, and coding support and has been covered for extensive EHR integrations and partnerships. In clinician trials, ambient drafts were strong, and the coding prompts were helpful. Health‑system buyers will appreciate its enterprise posture; ambulatory groups should review rollout timelines and training.
6. Tali AI: Canada‑Forward, Ambient Scribe with Public‑Sector Pilots
Tali shows momentum through Canada Health Infoway’s AI Scribe Program and provincial pilots in 2026, reflecting a focus on privacy, compliance, and primary care workflows. Clinicians we spoke with noted a quick learning curve. If you practice in Canada (PIPEDA), this is one to trial via funded programs.
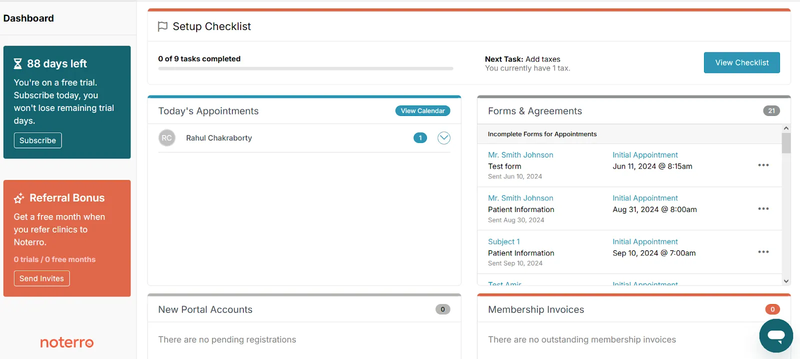
7. Noterro: Practice Management with Built‑In SOAP Notes (PT/Chiro/Massage)
Noterro is a practice‑management platform with SOAP charting and templates commonly used in PT, chiropractic, and massage therapy. It’s not a full ambient scribe, but if you need structured SOAP inside scheduling/billing, it’s a practical all‑in‑one. Pair with a dictation tool if you need voice. Software Advice review.
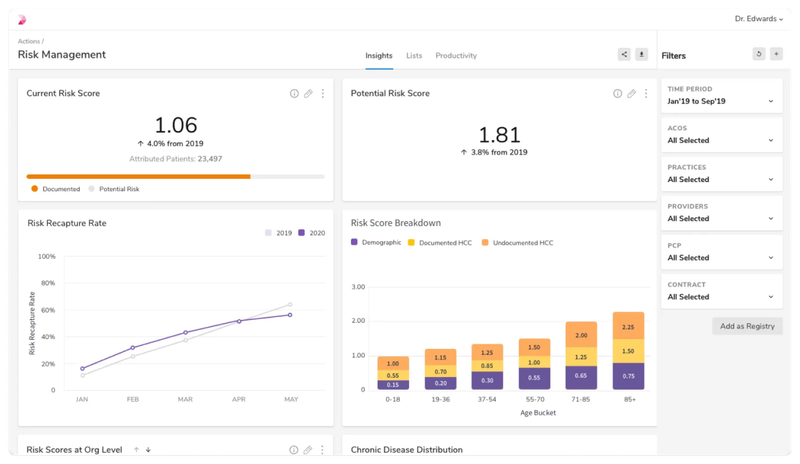
8. Innovaccer Copilot: Health‑System‑Grade AI Copilot with Ambient Scribe and gents
Innovaccer’s Provider Copilot appears in neutral trade coverage for launching AI agents and reporting documentation‑time reductions in early results. In our tests, note quality was solid; the platform angle (beyond just SOAP notes) suits integrated delivery networks. Validate EHR write‑back specifics and role‑based access before go‑live. Fierce Healthcare review.
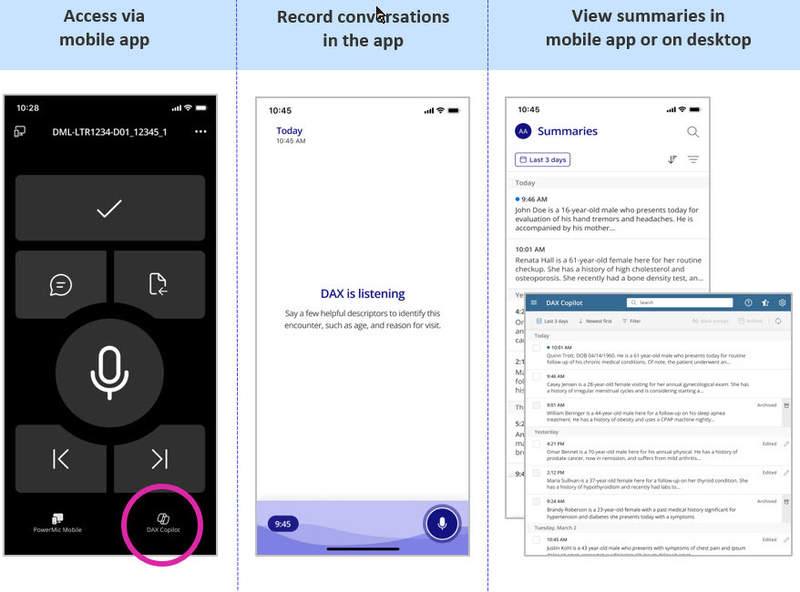
9. Microsoft Dragon Copilot (Nuance) - the Enterprise Default for Many Epic Sites
Microsoft’s ambient products, Dragon Copilot and DAX Copilot, are the most widely covered in major health systems, with studies and large‑scale deployments referenced by neutral outlets. If your system already standardizes on Dragon Medical One/DAX, this can be the path of least resistance; individual ambulatory practices may find procurement heavier than with SMB‑focused tools.
Top AI SOAP Note Tools: Quick Comparison (What Stood Out in Testing)
Tool | Best for | Strengths we observed | What to verify |
|---|---|---|---|
Twofold | Best all around for SMB practices and clinics | Accuracy, speed, reliability and simplicity | Support tiers |
Lindy.ai | Practices seeking agent‑style tasks + notes | Fast draft notes; broader admin automation ambitions | Independent evaluations; data governance & BAA |
DeepScribe | Specialty & enterprise | Ambient capture; specialty breadth | EHR write‑back fields; reporting |
Freed AI | Budget‑sensitive clinics | Very low friction; fast edits | PHI handling; audit trails |
Suki AI | Large ambulatory groups, hospitals | Mature ambient+dictation; coding assist | Integration timeline; training & support SLAs |
Tali AI | Canada (PIPEDA) primary care | Public pilot support; easy onboarding | Regional data residency; PIPEDA alignment |
Noterro | PT/chiro/massage practices | Built‑in SOAP in PM suite | Ambient voice needs add‑on |
Innovaccer Copilot | Health systems & IDNs | System‑level agents; early ROI signals | Role‑based access; EHR data mapping |
Microsoft Dragon Copilot | Epic‑heavy health systems | Scale, studies, adoption | Cost; device provisioning; consent workflows |
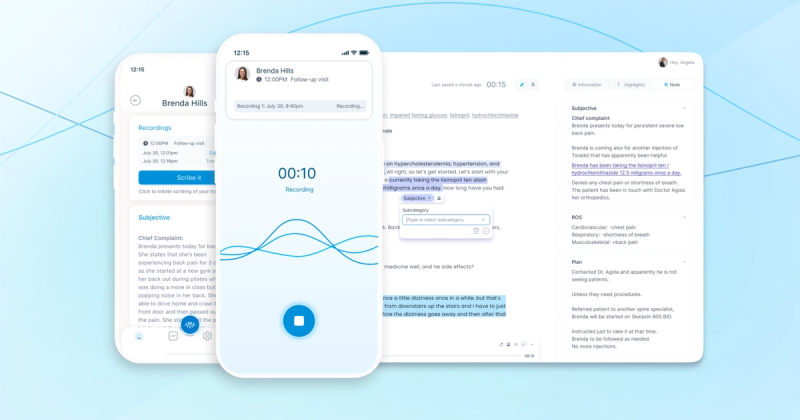
How AI SOAP Notes Work in Clinical Practice
Most “ambient scribe” tools follow a similar pipeline:
- Capture (consent → on‑device/app microphone)
- Transcribe (medical ASR)
- Summarize & structure into SOAP sections
- Draft orders/assessments/ICD hints (if enabled)
- Review & attest (clinician edits before EHR write‑back)
Peer‑reviewed and neutral reports consistently stress human review: AI scribes assist, clinicians remain responsible for the final note.
Why AI SOAP Notes Matter in 2026: Key Benefits
- Streamlining clinical workflows. Ambient tools trim note time and can reduce after‑hours charting; the magnitude varies by site and specialty.
- Reducing admin burden. Large programs report thousands of clinician hours saved, though ROI depends on local workflows.
- Improving patient outcomes (indirectly). Less screen time can improve patient engagement and reduce burnout risk associated with better safety and experience metrics.
- Enhancing accuracy & consistency. Modern systems filter small talk, recognize clinical language, and structure notes consistently - still with clinician oversight.
What to Look For in an AI SOAP Note Tool
- EHR & practice‑management integration. Verify your connector (FHIR/HL7/API), which fields the tool writes back (subjective/objective/diagnoses/orders), and how data lineage/audits work.
- HIPAA & PIPEDA compliance. Require a Business Associate Agreement (BAA) in the U.S.; in Canada, check PIPEDA obligations and data residency. Don’t rely on privacy‑policy language alone; OCR expects BAAs for tracking vendors, too.
- Customization for specialties. SOAP is universal; assessment and plan need specialty nuance (e.g., risk in psychiatry, functional goals in PT).
- Usability & learning curve. Time to “first usable note” should be minutes, not days; look for one‑tap corrections and quick template switches.
- Voice vs. typed input. Ambient capture should fall back to dictation and keyboard; some clinics prefer note‑from‑summary workflows over “always‑listening.”
- Pricing, trials, and flexibility. Favor time‑boxed pilots with clear success metrics (edit rate, minutes saved/visit) before committing.
AI SOAP Notes: Implementation Tips for Clinics
- Set up secure data access. Lock down PHI handling, confirm BAA, enable MFA, and review any analytics/“tracking tech” per updated OCR guidance.
- Train staff and manage change. Start with volunteer champions; standardize consent scripts; publish a one‑page “how we use ambient AI” for patients.
- Troubleshoot & support. Expect a few weeks of prompt/style tuning. Track edit reasons (e.g., missed ROS vs. incorrect meds) to guide vendor adjustments.
Common Mistakes to Avoid
- Relying fully on AI without review. Studies and regulators are clear: clinicians must review, edit, and attest to final notes.
- Using non‑compliant or unsupported tools. No BAA? No go. Be wary of tools using third‑party trackers or unclear data sharing.
- Ignoring staff training and feedback. Lack of change management is the top reason pilots stall.
- Overlooking customization. A one‑size template yields mediocre SOAP notes; insist on specialty‑aware outputs.
What’s Next for AI SOAP Note Tools?
More Ambient Voice Capabilities
Expect better speaker separation, on‑device redaction, and “room awareness” that captures clinically relevant exchanges while ignoring small talk.
Integration with Predictive AI
Vendors are beginning to surface coding suggestions, gap‑closure prompts, and evidence links during note drafting; enterprise copilots are expanding beyond documentation.
Interoperability Across EMRs and Platforms
Deeper EHR integrations and enterprise “copilots” continue, especially where voice, dictation, and ambient tools converge.
Greater Specialization (Therapy, PT, Psychiatry)
We’re seeing more domain‑specific templates and risk prompts tuned to mental health and rehab use cases.
Choosing the Right AI SOAP Note Tool in 2026
- Match capabilities to practice type. Therapists need risk language and progress note structure; primary care may prioritize med reconciliation, problem‑oriented assessments, and coding cues.
- Consider workflow compatibility. Document in‑room vs. after‑visit? Shared rooms? Noisy environments? Align tool mode (ambient, dictation, summary‑from‑transcript) with your day.
- Evaluate cost vs. time saved. Independent analyses show modest to meaningful time reductions; measure your own baseline and pick a plan that pays back within months. Peterson Health Technology Institute
- Look for transparent support & compliance. You want clear BAAs, audit trails, and responsive support—not just a demo sizzle reel. HHS.gov
- Prioritize solutions vetted by real clinicians. Favor tools with published studies, neutral coverage, or credible pilots at peer institutions.
How Twofold Simplifies AI SOAP Notes for Therapists with Smart, Secure Workflows
Twofold was built for mental and behavioral health. That means:
- Clinical‑ready SOAP outputs (e.g., formulation language, progress tracking, safety/risk elements)
- Fast onboarding for solos and small groups—no IT projects
- HIPAA compliance with BAAs and sensible defaults (MFA, least‑privilege access)
- Templates for therapy and psychiatry, plus quick edits for group visits and intakes
Learn more about how Twofold can support your AI SOAP note writing and have a look at our guide on how to make AI SOAP notes sound more human.
Final Take
If you remember only three things:
- Pilot with a purpose. Measure edit rate, minutes saved, and after‑hours charting deltas.
- Trust, then verify. Demand a BAA, confirm data flows, and pressure‑test EHR write‑back.
- Fit beats flash. The best AI SOAP note tool is the one that fits your clinic’s realities—patient mix, room dynamics, and staffing—not the one with the flashiest demo.
Frequently Asked Questions
ABOUT THE AUTHOR
Dr. Eli Neimark
Licensed Medical Doctor
Reduce burnout,
improve patient care.
Join thousands of clinicians already using AI to become more efficient.

The Future of Medical Transcription
Discover how AI scribes are revolutionizing medical transcription with real-time, accurate, and cost-effective documentation. Find out what’s next!

Can AI Notes Understand Therapy Work- Without Affecting The Relationship?
Explore how AI captures therapy notes while preserving human connection. Can the technology truly enhance the therapeutic alliance?

Integrating AI Therapy Notes with Your Telehealth Platform
Discover how to integrate AI therapy notes with your telehealth platform to streamline your EHR workflow.

