Cheat Sheet Hospice Documentation Template
Hey there, care coordinators and medical record mavens! Are you tired of the endless paper chase and constant puzzle‑solving when dealing with hospice documentation? Well, you're in the right place. Today, we're unpacking the medical code cheat sheet hospice documentation template, a handy tool designed to streamline your workload, reduce errors, and maybe, just maybe, save you a few gray hairs.
What Is a Hospice Documentation Template?
A hospice documentation template is a structured guide that aids healthcare professionals in accurately recording and tracking patient information. This tool simplifies the complex task of documenting a patient's hospice care journey, ensuring consistency and compliance with healthcare standards.
Primarily, these templates streamline workflows, reduce administrative burdens, and enhance communication among care teams. By utilizing predefined sections and coding standards, healthcare professionals can focus more on patient care rather than tedious paperwork.
Key Components of a Hospice Documentation Template
This template is composed of several essential elements that aid efficient documentation:
- Patient Identification Information
- Medical History and Current Diagnoses
- Treatment and Medication Plans
- Care Team and Contact Information
- Progress and Follow-up Notes
- Legal Documents and Consent Forms
How to Use a Hospice Documentation Template: Step-by-Step Process
Step 1: Begin with Patient Identification
Include the patient's name, date of birth, and unique hospital ID to secure all records under accurate identification.
Step 2: Record Medical History and Diagnoses
Enter a comprehensive review of the patient's past and current health conditions, which sets the stage for personalized care planning.
Step 3: Detail the Treatment Plan
Specify current treatments, medications, dosages, and any scheduled interventions that align with the patient’s end‑of‑life care wishes.
Step 4: Assemble the Care Team
Provide contact information for all involved healthcare providers to facilitate seamless communication and coordinated care efforts.
Step 5: Update with Progress Notes
Document clinical observations, treatment responses, and any changes in patient condition, maintaining an up‑to‑date overview of care.
Step 6: Attach Legal Documents
Secure and verify all necessary consent forms and legal documents relevant to hospice care mandates.
Benefits of a Hospice Documentation Template
Benefit | Description |
|---|---|
Consistency | Ensures uniform documentation across different healthcare providers. |
Efficiency | Streamlines time-consuming paperwork, allowing more focus on patient care. |
Error Reduction | Minimizes errors through predefined fields and coding assistance. |
Compliance | Helps maintain adherence to healthcare regulations and standards. |
Stakeholders in Hospice Documentation
Hospice documentation involves various stakeholders, each playing a pivotal role:
- Healthcare Providers: Doctors and nurses document patient's health progression. For example, a nurse updates the treatment response section during every visit.
- Coding Specialists: Ensure proper code assignments. They verify that the coding on the documents aligns with legal requirements, thereby avoiding costly errors.
- Administrative Staff: Manage data entry and record-keeping. They compile patient charts, ensuring the coordination of care is thoroughly documented.
- Patients and Families: Contribute to care decisions and provide personal information. For example, a family member signs the consent form confirming their understanding of the hospice plan.
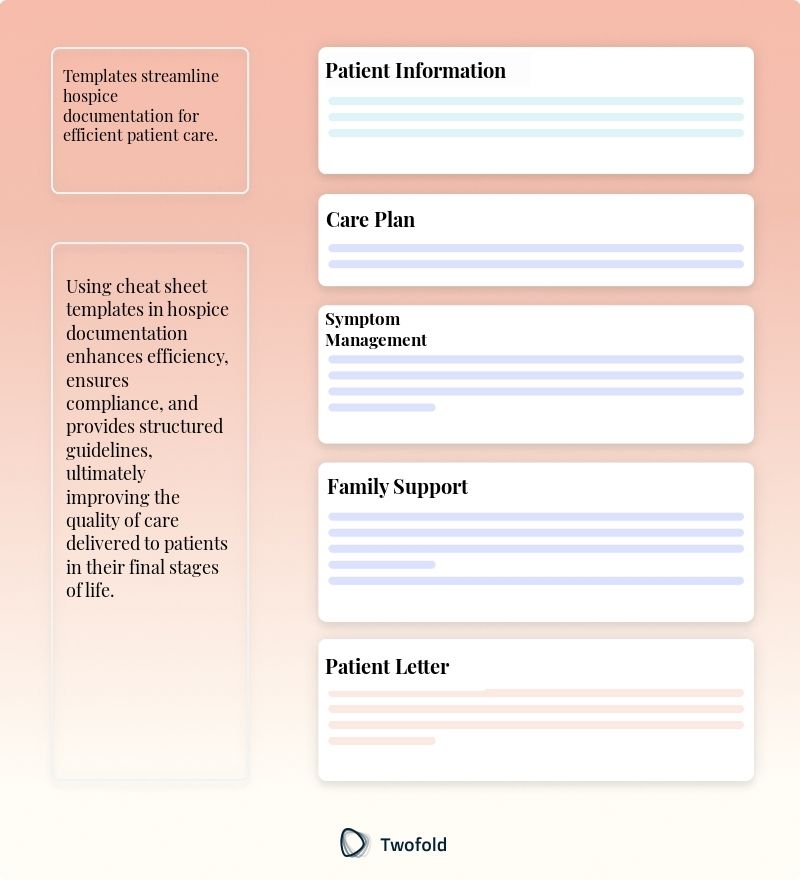
Example of a Hospice Documentation PDF
This PDF template serves as a practical example of how a hospice note is structured, offering real‑life applicability and immediate visual understanding.
Real-World Use Cases: Practical Impact of the Hospice Documentation Template
Hospice documentation templates make significant contributions to various healthcare settings. Here are some scenarios demonstrating their impact:
- In a busy urban hospital, a care team uses the template to quickly align on a new patient's hospice care strategy during a shift change.
- A coding specialist is able to verify all medical codes with a glance at the standardized template, preventing documentation discrepancies that could trigger audits.
- A rural healthcare clinic employs the template to maintain thorough documentation for remote consultations, thereby ensuring continuity of care despite geographic challenges.
Conclusion
Hospice documentation templates are indispensable tools in modern healthcare, easing the burden of paperwork, enhancing care consistency, and promoting effective communication. By employing such templates, healthcare providers can improve patient outcomes while efficiently managing their responsibilities. As you adopt hospice documentation templates, the potential to streamline your work and enrich patient care is boundless.
Disclaimer: This article is for informational purposes only and does not constitute legal or medical advice. Always consult professional guidelines and regulatory bodies for specific compliance requirements.

Dr. Danni Steimberg
Dr. Danni Steimberg is a pediatrician at Schneider Children’s Medical Center with extensive experience in patient care, medical education, and healthcare innovation. He earned his MD from Semmelweis University and has worked at Kaplan Medical Center and Sheba Medical Center.
When time is short and comfort is paramount, your hospice cheat sheet must surface the essentials instantly. The P.E.A.C.E. framework—Prognosis cue, Events timeline, Actions taken, Comfort level, Education given—keeps every entry focused, compassionate, and survey‑ready.
- Prognosis & Key Events: Start each note with a one-line prognosis update and the last critical change (“RR ↑, decreased oral intake”) so the whole team sees trajectory at a glance.
- Actions & Comfort Metrics: Log every intervention alongside a simple comfort score (0–10). Pairing morphine dose with pain relief proves efficacy and guides titration.
- Education & Family Alignment: Record the exact teaching points shared with caregivers (“signs of impending transition, med schedule”)—this not only meets CoP requirements but also reduces after-hours calls and documentation gaps.
Frequently Asked Questions
Reduce burnout,
improve patient care.
Join thousands of clinicians already using AI to become more efficient.
Daily Behavior Chart Template
Discover practical Daily Behavior Chart templates to enhance your documentation efficiency.

Client Feedback Form Template
Discover practical Client Feedback Form templates to enhance your documentation efficiency.

Living Well Template
Discover practical Living Well templates to enhance your documentation efficiency.

