
Progress Notes Template
Key Takeaways
- Progress notes are essential for documenting client interactions and treatment plans.
- They help mental health professionals track a client's progress over time.
- Templates ensure consistency and save time in the documentation process.
- Leveraging technology can enhance the efficiency of creating and managing progress notes.
What Is a Progress Note Template?
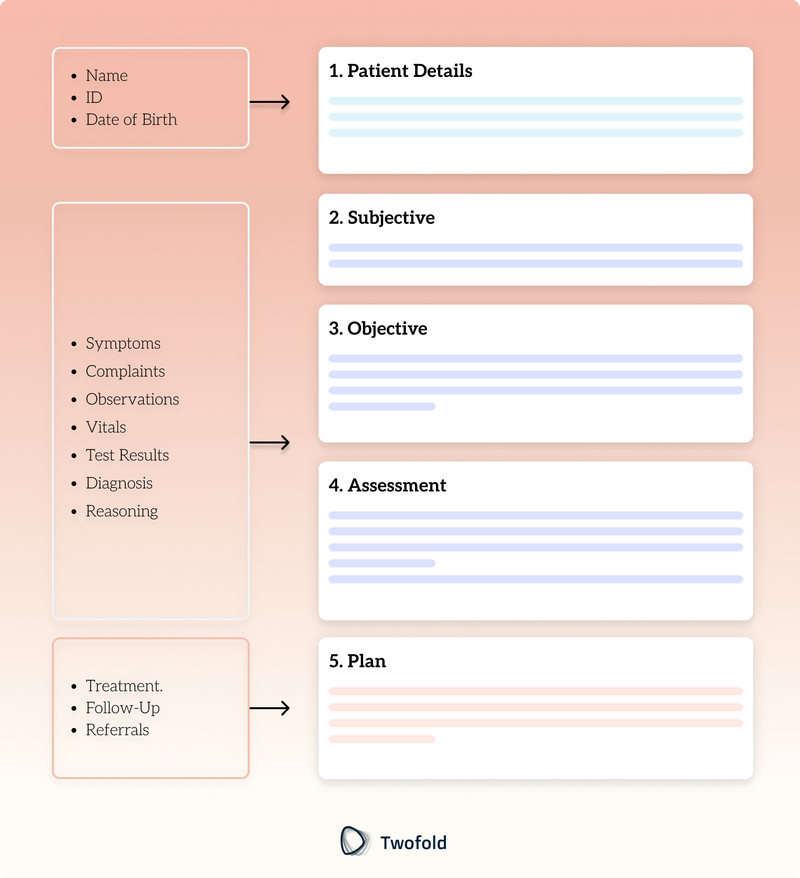
A progress note template is a standardized format that helps mental health professionals document client sessions efficiently. It typically includes key elements such as the client’s behavior, therapeutic interventions, response to treatment, and future plans. These templates ensure accurate and organized records, supporting effective treatment planning and continuity of care.
In addition to streamlining documentation, progress note templates promote consistency and compliance with professional and legal standards. They save time, help meet insurance or regulatory requirements, and reduce the risk of omitting critical details. Whether using pre‑designed formats or customizable options, these tools are essential for balancing quality care with efficient record‑keeping.
Key Components of a Progress Note
Progress notes are an essential tool for documenting therapy sessions in a clear and structured way. Below are the key components that ensure each note captures all relevant details for effective treatment planning and continuity of care:
- Identifying Information: Client's name, date of session, and therapist's name.
- Objective Observations: Clinician's observations of the client's behavior and mood.
- Therapeutic Interventions: Techniques and strategies used during the session.
- Client's Response: How the client reacted to the interventions.
- Plan for Future Sessions: Goals and strategies for upcoming therapy sessions.
How to Use a Progress Note Template: Step-by-Step Process
Step 1: Gather Client Information
Start by collecting the client's identifying information, such as their name, date of birth, and session date. This step is crucial as it establishes the context for the session and ensures that all documentation is correctly attributed to the right client. Make sure to verify the accuracy of the information to prevent any mix‑ups. Additionally, include any relevant background information that might impact the session, such as recent life events or changes in medication.
Step 2: Document Objective Observations
Note any observable behaviors or mood changes that occurred during the session. Pay attention to non‑verbal cues, such as body language and facial expressions, as they can provide valuable insights into the client's mental state. Consider the client's overall demeanor and any shifts from previous sessions. Documenting these observations helps in tracking the client's progress over time and identifying patterns that may require intervention.
Step 3: Record Therapeutic Interventions
Detail the interventions used and the client's response to these techniques. Include specific therapeutic strategies employed during the session, such as cognitive‑behavioral techniques, mindfulness exercises, or supportive counseling. Describe how the client engaged with the interventions, noting any resistance or enthusiasm. This information is critical for evaluating the effectiveness of the therapeutic approach and making necessary adjustments in future sessions.
Step 4: Outline Future Plans
Plan the next steps in the treatment process, including goals for future sessions. Establish clear, achievable objectives that align with the client's therapeutic goals. Consider incorporating feedback from the client to ensure that the treatment plan remains relevant and client‑centered. Outline any homework assignments or skills to practice before the next session, and schedule follow‑up appointments to maintain continuity of care.
Benefits of Progress Notes
Benefit | Description |
|---|---|
Consistency | Ensures all sessions are documented uniformly, which is crucial for maintaining a comprehensive record of the client's progress and therapeutic interventions. Consistent documentation helps mental health professionals track patterns and changes in the client's behavior over time, facilitating a more accurate assessment of treatment effectiveness. |
Efficiency | Saves time by providing a ready-to-use format that streamlines the documentation process. This efficiency allows therapists to focus more on the therapeutic process and less on administrative tasks, ultimately enhancing the quality of care provided to clients. Additionally, efficient documentation can help in quickly retrieving past notes, which is vital during follow-up appointments or when collaborating with other healthcare providers. |
Improved Communication | Facilitates information sharing with other healthcare providers, ensuring that all parties involved in a client's care are on the same page. This improved communication is essential for coordinating treatment plans, especially in cases where multiple professionals are involved. Shared progress notes can also aid in making informed decisions about the client's care, contributing to a more holistic approach to treatment. |
Legal Protection | Provides a detailed record of the treatment process for insurance purposes and legal protection. Comprehensive progress notes serve as evidence of the care provided, which can be crucial in the event of a dispute or audit. They also demonstrate the medical necessity of the interventions used, supporting claims for reimbursement from insurance companies. Legal protection through accurate documentation ensures that the therapist's actions are transparent and defensible. |
Example of a Progress Note Template
To better understand how progress note templates are structured, here is an example that outlines the key components commonly included:
How to Customize a Progress Note Template?
To customize a progress note template, consider the specific needs of your practice and client population. Here are some ways to tailor the template to enhance its effectiveness:
- Identify Practice Needs: Evaluate the unique requirements of your practice, such as the type of therapy sessions conducted, and adjust the template to reflect these needs.
- Client Population Focus: Adapt sections to cater to the demographics or specific issues prevalent among your clients, ensuring the template remains relevant.
- Incorporate Additional Sections: Add areas of focus like risk assessment, medication compliance, or family history to capture comprehensive information.
- Highlight Therapeutic Goals: Include sections that emphasize therapeutic goals and progress, allowing for a more targeted approach to treatment.
- Feedback Integration: Consider incorporating a section for client feedback to ensure the treatment plan is client-centered and responsive to their needs.
- Maintain Flexibility: Ensure the template allows for adjustments as therapeutic goals evolve, accommodating changes in the client's progress or treatment plan.
Leveraging Technology for Progress Notes
Integrating technology, particularly AI-powered tools, has transformed how mental health professionals document progress notes. These advanced tools can automate much of the data entry process, significantly reducing the time spent on paperwork. By streamlining documentation, they ensure that essential information, such as client behaviors, interventions, and responses, is captured consistently and accurately. This not only improves the quality of notes but also minimizes the risk of errors or omissions, which is crucial for effective treatment planning and maintaining compliance with professional standards.
Beyond efficiency, AI tools can provide valuable insights into the therapeutic process. Some platforms analyze session data to identify trends or patterns, helping clinicians tailor interventions more effectively. Additionally, they often include features like customizable templates and compliance checks, ensuring notes meet insurance and regulatory requirements. By leveraging such technology, mental health professionals can allocate more time to direct client care, enhancing the overall therapeutic experience.
Conclusion
Progress note templates are invaluable tools for mental health professionals, offering a structured approach to documenting client interactions and treatment plans. By using these templates, clinicians can enhance the efficiency and effectiveness of their clinical documentation, ultimately improving client outcomes.
For advanced solutions in medical documentation, explore our AI medical scribe services, designed to revolutionize how you create and manage your clinical notes.
Disclaimer: This article is for informational purposes only and does not constitute legal or medical advice. Always consult professional guidelines and regulatory bodies for specific compliance requirements.

Michael Tzach
Michael is a tech leader with expertise in health tech, specializing in innovative software solutions that enhance healthcare efficiency and compliance.
- Align with Therapy Style: Pick templates that fit your clinical approach, like BIRP for behavioral focus or SOAP for structured care.
- Focus on Key Details: Customize sections to capture client goals and measurable outcomes clearly.
- Use Smart Tools: Incorporate AI to speed up note-taking and ensure accuracy.
Frequently Asked Questions
Reduce burnout,
improve patient care.
Join thousands of clinicians already using AI to become more efficient.

Superbill Template
Discover practical Superbill templates to enhance your documentation efficiency.

EMDR Note Template
Discover practical EMDR progress note templates to enhance your documentation efficiency.

Mental Health Intake Assessment Template
Discover practical Mental Health Intake Assessment templates to enhance your documentation efficiency.


